Abstract
Gastrointestinal (GI) adverse effects are the dose limiting toxicity of high-dose melphalan (HDM), and despite prophylactic measures, continue to have a significant impact on morbidity, length of stay, and quality of life. There are limited contemporary data on gastrointestinal toxicity associated with HDM. Our objective was to characterize the GI toxicity of HDM and identify risk factors for severe toxicity in a cohort of patients.
We conducted a retrospective study on 100 consecutive patients with multiple myeloma, amyloidosis, or lymphoma who underwent autologous stem-cell transplant at Columbia University Irving Medical Center using HDM, either alone or in combination with other chemotherapeutic agents. Gastrointestinal adverse events, use of rescue medications, infectious complications, and length of stay were collected from electronic medical records. CTCAE (Common Terminology for Adverse Events) grading for GI events was conducted daily. Risk factors for GI toxicity were identified using linear regression and then examined in a multivariable model.
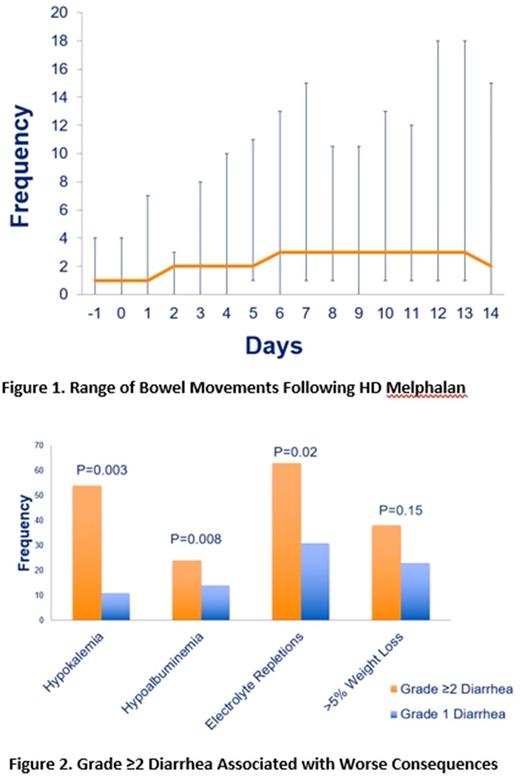
Patients (median age 56 years, range 20-73) had myeloma (42%), lymphoma (42%), or amyloidosis (16%). Melphalan dose was 200 (40%), 140 (59%), or 100 mg/m2 (1%). Ninety-seven percent of patients experienced diarrhea ranging 1 - 18 daily bowel movements (Figure 1) and lasting 0 - 17 days (median 7). Nausea and vomiting of any grade occurred in 88% and 61% of patients, respectively. Sixty-two percent developed grade≥2 diarrhea, and grade≥2 nausea and vomiting was observed in 35% and 7%, respectively. The mean total number of bowel movements during a 14-day period post-transplant was 39 (maximum 67). Rescue loperamide was given 10 doses on average overall (range 0-43). Eighteen percent experienced weight loss of more than 10% and 38% dropped albumin level by at least 1g/dL.
Patients with grade≥2 diarrhea had a higher incidence of hypokalemia, hypoalbuminemia, required greater electrolyte repletions (Figure 2), utilized more rescue medications, and had prolonged diarrhea (average 8.7 v. 5 days, p<0.0001) compared to patients with grade 1 diarrhea. Patients with grade≥2 diarrhea were also more likely to stay in the hospital more than 23 days (p=0.07). Of the entire cohort, eleven percent had at least one episode of incontinence and 15% had an infection identified in stool studies. To rule out further complications, 31% of patients had CT scans of the abdomen and pelvis but only 8% showed evidence of colitis.
Grade≥2 diarrhea was independently associated with age>50 years (p=0.04), creatinine clearance <60 ml/min (p=0.05), and female sex (p=0.04). Female sex was also associated with developing grade≥1 nausea (p=0.05) and vomiting (p=0.09). Melphalan dose, underlying disease, and HDM v. BEAM (BCNU, Etoposide, Ara-C, Melphalan) were not significantly associated with diarrhea severity, although numerically there were more patients with grade≥2 diarrhea in the HDM 200 mg/m2 compared to 140 mg/m2 (70% vs. 59%).
Diarrhea remains a very common side effect of HDM with no improvement over historical rates and no known prophylactic measures. Female sex, a low creatinine clearance, and age over 50 years portend a higher risk for severe diarrhea, and female sex for nausea and vomiting. Novel therapies for chemotherapy-induced diarrhea are critically needed for patients undergoing stem-cell transplantation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal